WHAT IS SUPPORTIVE AND PALLIATIVE CARE?
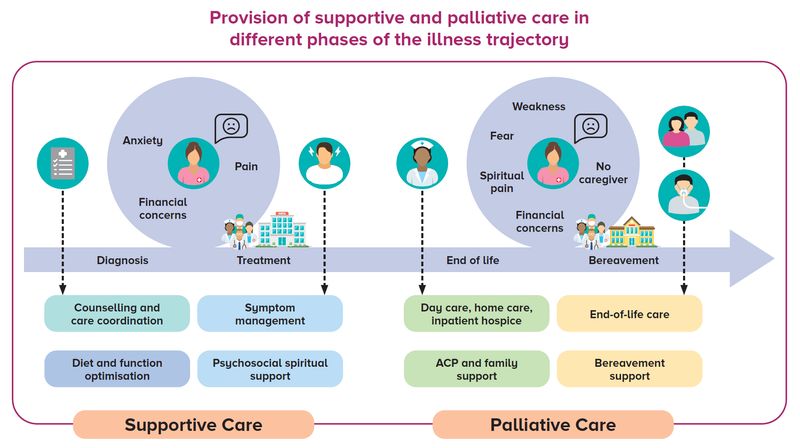
With our ageing population and improved survival brought about by medical advancements, the number of
people living with serious life-threatening illnesses is ever increasing. To help them maintain their quality of life
while managing illness- or treatment-induced symptoms, it is important to ensure that supportive and palliative
care is available in different phases of the serious illness trajectory.
Supportive care focuses on providing patients
and families with the appropriate support to allay
concerns relating to illness and make lifestyle
changes to improve their quality of life while living
with the illness.
This can be introduced as early as the point of diagnosis
of a serious life-limiting illness, regardless of the stage
of illness and treatment status.
Palliative care focuses on optimising quality of
life through relieving symptoms and addressing
psychosocial issues, preparing and supporting family
and caregivers for the end of life, advance care
planning (ACP) as well as bereavement support.
Currently, less than half of the seriously ill patient
population in Singapore is introduced to specialist
palliative care services and often at very late in their
illness trajectory, for symptom management prior to
death.
Some serious illnesses include:
-
End-stage lung, heart, renal and
neurodegenerative diseases
- Advanced dementia and frailty
- Cancer
A joint effort of shared care
While there is a need to increase access to supportive
and palliative care, it is important to recognise the
collective effort required to provide such care across
the different care settings.
In acute hospitals, generalist supportive and palliative
care can be provided by primary teams as part of their
specialty care with sufficient training and guidance,
before referring patients to palliative care specialists
for complex care needs.
Generalist supportive and palliative care can also be provided in the primary care setting, to ensure
patients with serious illnesses continue to live well
in the community.
THE SINGHEALTH DUKE-NUS
SUPPORTIVE & PALLIATIVE CARE CENTRE
Established in April 2020, the SingHealth Duke-NUS Supportive & Palliative Care Centre (SDSPCC) brings together healthcare professionals of different expertise, dedicated to improving the quality of and access to
supportive and palliative care for patients and their caregivers. It also fosters collaboration with community
partners to achieve coordinated care and the best patient outcomes.
There are currently ten supportive and palliative care services across SingHealth institutions:
Singapore General Hospital
Changi General Hospital
Sengkang General Hospital
KK Women’s and Children’s Hospital
(Paediatric and Gynae-Oncology)
National Cancer Centre Singapore
National Heart Centre Singapore
National Neuroscience Institute
- Inpatient Hospice Palliative Care Services
(IHPCS) at Outram Community Hospital and
Sengkang Community Hospital
CLINICAL SERVICES
Inter-professional clinical care
Working in inter-professional clinical care teams
consisting of doctors, nurses, medical social workers
and other allied health professionals, SDSPCC
provides different aspects of specialist palliative
care in inpatient, outpatient and community settings.
Inter-department collaborations
Inter-department collaborations have been established
by respective palliative care services to help clinicians from different specialties identify eligible
patients earlier in their illness trajectory. Advice is
also given to help primary teams provide generalist
supportive and palliative care in their practice, prior
to referral to palliative care specialists for patients with more complex palliative care needs.
Harmonisation of care
Dedicated to improving the quality of palliative care,
SDSPCC is currently leading the harmonisation of
the clinical assessment tools under the Palliative
Care Outcomes Collaboration within SingHealth.
We aim to standardise palliative care clinical service quality indicators for cluster, national and
international benchmarking.
COMMUNITY PARTNERSHIPS
As the supportive and palliative care needs of
patients and caregivers vary in intensity over time, it
is important that patients are rightly sited in different
care settings based on their needs. The level of
care provision increases along primary, acute,
intermediate and long-term care settings.
Frequent visits to hospitals and the transition to
step-down care are also pain points for patients with
serious illnesses and their caregivers. SDSPCC is
working to establish collaborations with community
partners, including hospices and community
hospitals, to facilitate smooth and seamless care
transitions while ensuring consistent quality of care
across different care settings.
EDUCATION
Training programmes
Beyond central planning, SDSPCC works closely
with the Lien Centre for Palliative Care (LCPC)
and Singapore Hospice Council (SHC) to develop
generalist supportive and palliative care training programmes for healthcare providers, students,
community providers and the public, as well as to
develop caregiver resources. For more information
on generalist supportive and palliative care courses
for general practitioners (GPs), please refer to
Table 1.
Graduate Diploma in Palliative Medicine | 10 months of part-time generalist training offered by the Division of Graduate Medical
Studies, NUS Yong Loo Lin School of Medicine, aimed at training physicians who are
interested in palliative care with the required competency and confidence to manage
patients with palliative care needs in their respective care settings. The course involves a mix of self-study, seminars with group discussions, group learning and six full-day attachments in various palliative care settings. Learners will also be assigned to a supervisor (specialist in palliative medicine). |
Post-Graduate Course in Palliative Medicine (LCPC-SHC) | A 3-day course by LCPC and SHC on the principles and practice of palliative medicine for physicians across all settings. It aims to equip participants with generalist palliative care skills and knowledge for integration into their practice in the care for patients with life-limiting illnesses. |
Renal Supportive Care Course (Interdisciplinary) | A 3-day online course conducted by LCPC to equip healthcare professionals caring for advanced chronic kidney disease patients with basic supportive care skills and knowledge to integrate into their practice. |
Table 1 Generalist supportive and palliative care courses for doctors in Singapore
Competency frameworks
SDSPCC has also developed competency frameworks
for nurses and medical social workers to
enhance their skills and competencies within the
palliative care fraternity, which will be shared with
the Ministry of Health to aid development of national
competency frameworks in palliative care.
Existing training programmes available are also
mapped to performance expectations to facilitate
the development of individuals within the competency
framework.
Public education
In public education, the National Cancer Centre Singapore (NCCS) and Singapore General Hospital
(SGH) have provided supportive survivorship care
education to SingHealth Polyclinics, SingHealth
Community Nursing, as well as volunteers and
community social workers in selected social service
agencies (e.g., Breast Cancer Foundation, SPD, SG
Enable and Singapore Cancer Society).
NCCS also conducts an annual Supportive and
Survivorship Care Symposium targeting healthcare
professionals, patients and caregivers to share the
latest updates on cancer supportive care.
RESEARCH
SDSPCC aims to train more healthcare professionals
in research, encourage cross-institution
collaboration, embrace innovation and experiment
with new models of care.
There are plans to develop a SingHealth Palliative
Care Registry – a database that can be used to
address service development, quality improvement
and research objectives. The registry will eventually
be linked to data available in the hospices and
home care services in the community, to track the
patient journey from hospital to community and monitor care outcomes.
The team is exploring the possibility of providing
‘precision medicine’ in the field of supportive
and palliative care to achieve more efficient and
effective models of care. This involves identifying
individualised patient needs through data in
electronic health records or patient-reported
outcome measures, and matching them with the
specific support required to meet those needs.
Our Services
Domains of care
-
Prevention, assessment and management of
pain and other symptoms (e.g., shortness of
breath, loss of appetite, nausea or vomiting) related to serious illnesses and their treatments
- Patient and family/caregiver education
- Emotional, psychological and spiritual support
- Practical and social support
- Care and discharge planning
- End-of-life and bereavement care
Some inter-department collaborations
within SingHealth
-
Internal Medicine
- Geriatric Medicine
- Intensive Care Unit
- Haematology
- Oncology
- Cardiology
- Neonatology / Paediatrics
For referral to palliative care services, please contact the respective institutions:
Singapore General Hospital: 6326 6060
Changi General Hospital: 6788 3003
Sengkang General Hospital 6930 6000
KK Women’s and Children’s Hospital: 6692 2984
National Cancer Centre Singapore 6436 8288
National Heart Centre Singapore 6704 2222
National Neuroscience Institute 6330 6363
GPs who would like to collaborate with the SingHealth Duke-NUS Supportive & Palliative Care Centre,
please email to sdspcc@singhealth.com.sg.
Our Executive Committee
Head
1. Clin Asst Prof Patricia Neo
Senior Consultant,
Division of Supportive & Palliative Care, NCCS
Deputy Head (Clinical Services/Education)
2. Clin Asst Prof Alethea Yee
Senior Consultant,
Division of Supportive & Palliative Care, NCCS;
Clinical Director,
Assisi Hospice;
Director of Education,
Lien Centre for Palliative Care, Duke-NUS Medical School
Deputy Head (Research)
3. Prof Eric Finkelstein
Executive Director,
Lien Centre for Palliative Care, Duke-NUS Medical School;
Professor,
Health Services and Systems Research, Duke-NUS Medical School
Strategic Advisor, Community Partnership
4. Ms Irene Chan
Director,
Office of Patient Experience, KKH
Director, Clinical Services
5. Clin Asst Prof Shirlynn Ho
Senior Consultant,
Division of Supportive & Palliative Care, NCCS
Director, Community Partnership
6. Dr Lee Guozhang
Consultant,
Internal Medicine Supportive and Palliative Care Service,
Department of Internal Medicine, SGH
Director, Education
7. Clin Asst Prof Peh Tan Ying
Senior Consultant,
Division of Supportive & Palliative Care, NCCS;
Head (Medical),
Assisi Hospice
Director, Research
8. Asst Prof Grace Yang
Senior Consultant,
Division of Supportive & Palliative Care, NCCS;
Assistant Professor,
Lien Centre for Palliative Care, Duke-NUS Medical School
Programme Director (Medical), Clinical Services
9. Dr Komal Tewani
Senior Consultant,
Department of Gynaecological Oncology, KKH;
Head,
Women’s Palliative Care Service, KKH
Programme Director (Allied Health), Clinical Services
10. Assoc Prof Lita Chew
Group Director,
Group Allied Health, SingHealth
Programme Director (Nursing), Clinical Services
11. Ms Wong Yoke Ping
Senior Nurse Manager,
Specialty Nursing, CGH
Co-Director, Community Partnership
12. Clin Asst Prof Loo Yuxian
Head of Service & Consultant,
Post-Acute and Continuing Care, SCH@OCH
Co-Director, Education
13. Mr Andy Sim
Principal Medical Social Worker (Educator),
Medical Social Services, SGH
Co-Director, Research
14. Dr Ling Xu Yi
Principal Clinical Pharmacist,
Pharmacy, KKH
ADDITIONAL RESOURCES
Singapore Hospice Council
-
Referral to Community Palliative Care Services in Singapore (SHC Common Referral Form)
- 2021 Singapore Hospice Council FAQs on Palliative Care
Lien Centre for Palliative Care
- SG Pall eBook
- Training and Courses
